Abstract
Introduction: Vaso-occlusive pain crisis (VOC) are the hallmark of sickle cell disease (SCD) and the primary reason for which affected individuals seek acute care (Boussard et al JAMA, 2010). Both national and international guidelines recommend aggressive IV opioids, intravenous fluids and anti-inflammatory therapy as the mainstay of treatment for acute SCD pain. In an effort to avoid acute care for VOC, many pain crises are managed at home with oral agents, including anti-inflammatory and opioid medications. However, there are no current guidelines on the use and type of medications for home pain management, likely due to lack of clinical trials comparing the efficacy and safety of oral agents for use at home. Previous studies suggest geographic differences in the use of opioids for home pain management (Kanter et al, Br J Haem, 2018). Amplifying these issues is the growing concern for opioid abuse and misuse both in the US and internationally (WHO, 2013). This study aimed to describe the opioid prescribing habits among international providers treating individuals with SCD, to better assess the different medications used for outpatient management of SCD-related pain both in the United States (US) and internationally.
Methods: A thirty-question REDcap survey was disseminated electronically. Participants were recruited using a combination purposive and snowball sampling strategy. Providers were initially identified by email using databases from SCD conferences. After the initial responses were received, responding participants were asked to refer other providers who treat SCD.
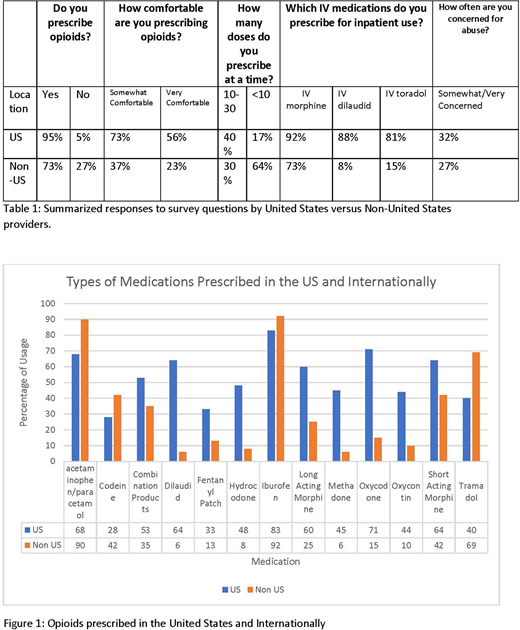
Results: There were 17 countries represented. Over half of the respondents were from the US (59%,75/127). Most of the respondents were Hematologist/Oncologists both pediatric-focused (43%, 54/127) and adult-focused (34%,44/127). Providers from the US were more likely to prescribe opioids than non-US physicians (95% vs 73%, p<.001) and were more likely to be "very comfortable" prescribing opioids than non-US physicians (73% vs 37%, p<.001). In exploring the rationale of physicians that do not prescribe opioids for outpatient management of pain, non-US physicians were more likely to site "outpatient opioids not being allowed" (50%) vs 25%), although this was not significant. Of those physicians who prescribe opioids, most (70%) prescribed 30 doses or less at a time. However, non-US physicians were more likely to prescribe less than 10 doses at a time (64%vs 17%, p <.001). Overall, the top 5 most commonly prescribed medications for home pain management were; acetaminophen/paracetamol (98%), ibuprofen (88%), short acting morphine (55%), tramadol (52%) and oxycodone (48%). Non US physicians were more likely to prescribe acetaminophen/paracetamol (90%vs 68%, p<.05) and tramadol (69% vs 30%, p <.05), while US providers more likely to prescribe short acting morphine (64% vs 42%, p<.05), long acting morphine (60% vs 25%, p<.001), oxycodone (70% vs 15%, p<.001), oxycontin (44% vs 10%, p<.001) and dilaudid (64% vs 6%, p<.001). The most commonly ordered acute care parenteral medications were morphine (84%), dilaudid (55%) and Toradol (54%). Parenteral dilaudid was used almost entirely in the US alone (88% vs 8%, p<.001). US physicians were more likely to be concerned that patients were abusing opioids than non-US physicians (32% vs 27%, p<.05).
Discussion: Acute vaso-occlusive pain episodes are the most common reason for healthcare utilization in SCD. Although many countries use oral opioids for outpatient pain management, the majority of non-US prescribers are more likely to prescribe less potent opioids in lower quantities. Non-US physicians are more likely to use Tylenol and NSAIDS before opioids, with Tramadol being prescribed most often. As concerns have increased for opioid-induced hyerpalgesia and other complications of long term opioid use, alternative disease-modifying agents for the prevention of SCD related pain remain a huge unmet need. However, identifying optimal home pain management strategies is also necessary to improve care in SCD. Finally, as more multinational studies of novel therapeutics are undertaken in SCD, it is important to note the significant geographic differences in medication prescribing both at home and in the hospital and to work to create multinational guidelines on outpatient management of VOC's.
Kanter:bluebird bio: Membership on an entity's Board of Directors or advisory committees, Research Funding; AstraZeneca: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding; ASH: Membership on an entity's Board of Directors or advisory committees; Apopharma: Research Funding; Pfizer: Research Funding; NHLBI: Membership on an entity's Board of Directors or advisory committees, Research Funding; Global Blood Therapeutics: Research Funding; Sancilio: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal